Most of the time, it’s from gallstones or drinking too much alcohol. But, some medicines, infections, and genes can also cause it. People with pancreatitis may feel a lot of stomach pain, throw up, and have a fever.
To figure out if someone has this problem, doctors do tests and take pictures. They want to help the pancreas heal and deal with any problems. This might mean staying in the hospital, taking medicine for pain, and eating differently. To stop it from happening again, they might tell you to stop drinking or get rid of gallstones.
What is Pancreatitis?
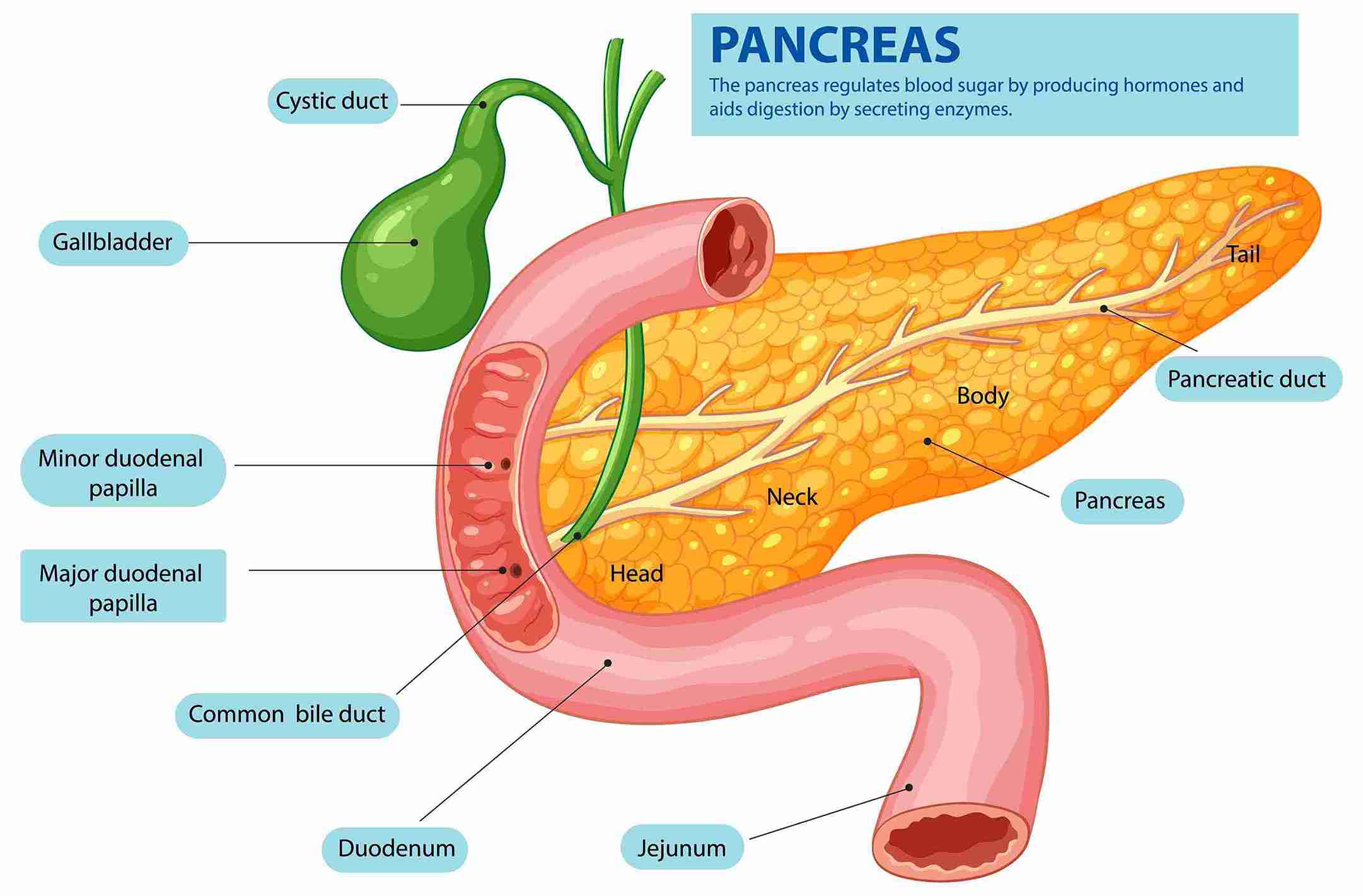
Pancreatitis is when the pancreas gets inflamed. This gland is behind the stomach. It makes enzymes for digestion and hormones like insulin to control blood sugar.
Knowing about acute pancreatitis and chronic pancreatitis helps us understand this condition. It’s key to getting the right treatment.
Acute Pancreatitis
Acute pancreatitis is a sudden, severe inflammation. It usually doesn’t last long and might get better by itself. But, it can be very serious if not treated.
It often happens because of gallstones or drinking too much alcohol.
Chronic Pancreatitis
Chronic Pancreatitis is a long-term inflammation. It can damage the pancreas for good. This makes it hard for the pancreas to work right.
It can come from having many episodes of acute pancreatitis. Or it could be from other health issues.
Causes of Pancreatitis
The main causes are gallstones and heavy alcohol use. Gallstones can block the bile duct. This stops pancreatic enzymes from going to the small intestine. They then go back to the pancreas, causing irritation and inflammation.
Gallstones Related
Gallstones often lead to gallstones pancreatitis. When they block the bile duct, they stop pancreatic enzymes from going to the small intestine. This makes the enzymes work in the pancreas, causing inflammation and causes of pancreatitis.
Alcohol-Induced
Drinking too much alcohol can hurt pancreatic cells. It can also make digestive enzymes work too early. This makes the pancreas inflamed and swollen, causing a lot of stomach pain.
Other Causes
Other reasons include some medicines, high triglyceride or calcium levels, infections, trauma, and genetics. Sometimes, the cause is not found, known as idiopathic pancreatitis.
Symptoms of Pancreatitis

The main symptom is very bad stomach pain. Acute pancreatitis can also cause feeling sick, throwing up, a fast heart rate, and a fever. The pain might spread to the back or chest and gets worse after eating.
*Chronic pancreatitis* leads to ongoing stomach pain, trouble digesting food, and getting fatty, oily stools. You might also lose weight without trying, and your blood pressure could drop.
Symptoms of pancreatitis can change in strength and may come and go. But, you must get medical help fast. *Pancreatitis symptoms* can be mild or very bad. It’s important to see a doctor to find out what’s wrong and get treatment.
*Acute pancreatitis symptoms* can come on suddenly and be very strong. *Chronic pancreatitis symptoms* can get worse over time. But, pancreatitis is a serious issue. You should get medical help quickly to manage the symptoms and avoid more problems.
While pancreatitis primarily affects the digestive system, severe metabolic disturbances associated with this condition can lead to hypercalcemia, which in turn increases the risk of bladder calculi formation due to elevated calcium levels in the urine.
Diagnosing Pancreatitis
Getting a correct diagnosis is key to getting better. Doctors start by checking the patient’s health and past illnesses. They also look at blood tests to see if pancreatic enzymes are high.
Imaging Tests
Tests like X-rays, ultrasounds, and CT scans help too. They show the pancreas and what’s around it. This helps doctors find out why and how bad it is.
Magnetic resonance cholangiopancreatography (MRCP) also helps. It makes detailed pictures of the bile and pancreatic ducts. Sometimes, doctors use endoscopic retrograde cholangiopancreatography (ERCP) too. This test looks at the ducts through a tube in the mouth. It’s good for finding things like gallstones or blockages.
Treatment
The main aim of treatment is to help the pancreas heal. For acute pancreatitis, patients often go to the hospital. They get fluids through a vein, painkillers, and might get antibiotics too.
They might not eat or drink for a bit to help the pancreas heal. In serious cases, they might need a feeding tube or surgery. This could be to drain fluids or remove gallstones or the gallbladder.
Treating Acute Pancreatitis
First, acute pancreatitis treatment aims to rest the pancreas and ease symptoms. This means going to the hospital, getting fluids through a vein, and taking painkillers. Sometimes, antibiotics are given to prevent infections.
Patients might not eat or drink for a while to help the pancreas heal.
Treating Chronic Pancreatitis
For chronic pancreatitis, treatment is about managing pain and helping with digestion. Doctors might give medicines, enzyme supplements, and suggest changes in diet. In some cases, surgery is needed to remove damaged parts of the pancreas.
The goal is to make symptoms better and stop more damage to the pancreas. A cholesterol-lowering diet plan can be beneficial in managing pancreatitis, as reducing dietary fats can help decrease the risk of triggering inflammation in the pancreas.
Risk Factors for Pancreatitis
Some things can make it more likely to get pancreatitis. Knowing these pancreatitis risk factors helps in staying healthy. It’s key to understand them.
Drinking a lot of alcohol is a big risk for pancreatitis. If you drink four or five drinks a day, you’re more likely to get it. Smoking also makes it worse by harming the pancreas.
Being overweight, having diabetes, or a family history of pancreatitis are risks too. Other risks include gallstones, high blood triglycerides, high calcium levels, and cystic fibrosis. Some medicines can also raise the risk.
By knowing these pancreatitis risk factors, you can prevent it. Going to regular doctor visits, living a healthy life, and managing health issues can help. This can lower your chance of getting pancreatitis.
Pancreatitis can significantly impair the digestive system’s function, and maintaining adequate levels of Vitamins, particularly fat-soluble ones like A, D, E, and K, is crucial for supporting digestive health and mitigating nutrient malabsorption.
Complications
Pancreatitis can be serious and even life-threatening if not treated. It’s important to know about these risks to take care of your health.
Acute Pancreatitis Complications
A severe case of acute pancreatitis can cause the pancreas to die and get infected. This can lead to sepsis and failure of many organs. It might also create a pancreatic pseudocyst, which can get infected or burst, causing more problems.
Chronic Pancreatitis Complications
People with chronic pancreatitis might not digest food well, leading to poor nutrition and losing weight. They could also get diabetes because the pancreas can’t make insulin right. Other issues include ongoing pain, blocked pancreatic ducts, and a higher chance of getting pancreatic cancer.
Pancreatitis Prevention
Preventing pancreatitis means looking at the main causes and reducing the risk factors. If you’ve had pancreatitis from gallstones, getting your gallbladder removed can stop more problems. If alcohol caused your pancreatitis, don’t drink alcohol anymore to reduce the risk of recurrence.
Keeping a healthy weight, managing diabetes, and avoiding certain medicines are key steps. Regular doctor visits can spot and fix risk factors early.
By acting early to prevent pancreatitis, you can greatly cut down the chance of this severe issue. Fixing the main causes and living healthily are big steps in reducing the risk of pancreatitis.
Living with Pancreatitis
Living with pancreatitis is tough, but many people manage well. For those with chronic pancreatitis, it’s all about controlling pain and managing diabetes. They also focus on replacing digestive enzymes.
Eating small, low-fat meals can ease the pancreas’s workload. Sometimes, you might need painkillers and enzyme supplements. It’s important to see a doctor regularly to keep an eye on things.
Having support from loved ones and mental health experts helps a lot. They can help with the tough parts of living with pancreatitis. With the right support and attitude, many people lead happy, active lives despite their condition.
Conclusion
Understanding pancreatitis is key to managing it well. Knowing the causes, like gallstones and alcohol, helps. It also helps to know the symptoms and possible problems.
Getting the right diagnosis and treatment is important. This is true for both sudden and ongoing pancreatitis. Working with doctors and following their advice is crucial.
By making healthy choices, like eating right and staying active, many people with pancreatitis can feel better. They can live a good life.
Preventing pancreatitis is also important. Knowing what increases the risk helps. Avoiding too much alcohol and keeping a healthy weight are good steps.
Addressing any health issues you have is also key. Taking these steps can lower your chance of getting pancreatitis.
FAQ’s
What is pancreatitis?
Pancreatitis is when the pancreas gets inflamed. The pancreas is behind the stomach. It helps with digestion and making insulin. It can be sudden and short or last a long time, causing damage.
What are the most common causes of pancreatitis?
Gallstones and drinking too much alcohol are the top causes. Other reasons include some medicines, high blood fats, infections, and injuries. Some people might get it because of their genes.
What are the symptoms of pancreatitis?
The main symptom is very bad stomach pain. If it’s sudden, you might feel sick, throw up, have a fast heart rate, and a fever. If it’s ongoing, you might lose weight, have trouble digesting food, and feel weak.
How is pancreatitis diagnosed?
Doctors use a physical exam, your health history, and tests to diagnose it. They check for high levels of certain enzymes in your blood. They might also use X-rays, ultrasounds, CT scans, and MRCP images.
How is pancreatitis treated?
The main goal is to help the pancreas heal. For sudden cases, you might need to stay in the hospital. You’ll get fluids through a vein, medicine for pain, and maybe antibiotics.
For ongoing cases, doctors help manage pain and replace digestive enzymes. They also work on stopping the cause, like helping you quit drinking.
What are the risk factors for pancreatitis?
Drinking a lot of alcohol, smoking, being overweight, having diabetes, and a family history increase your risk. Gallstones, high blood fats, some medicines, and conditions like cystic fibrosis can also raise your chances.
What are the potential complications of pancreatitis?
Serious cases can lead to serious problems like infection and damage to the pancreas. It can also cause sepsis and failure of other organs. Long-term, it can lead to diabetes, chronic pain, and an increased risk of cancer.
How can pancreatitis be prevented?
To prevent it, focus on the main causes and risk factors. This means removing the gallbladder for some, not drinking alcohol, staying at a healthy weight, and avoiding certain medicines.
What is it like to live with pancreatitis?
It can be tough, but many people manage their symptoms well. This might mean eating differently, taking medicine, seeing your doctor often, and getting support from loved ones and mental health experts.